Our Services
| Craniosynostosis & Facial Asymmetry | ||
|---|---|---|
Craniosynostosis & Facial Asymmetry
CraniosynostosisCraniosynostosis implies that early synostosis of cranial suture resulting in the cessation of the bony growth and disturbing the normal growth of the head eventually. If it is severe or is left untreated for a long time, cranium may be pressed and development of brain can be bothered and visual impairment and mental retardation may follow and even the life can be threatened. Deformity of head and face may have adverse effect on the child’s social activity and personality development. Early diagnosis and appropriate intervention of the craniosynosis can prevent the functional impediment and ensure one’s normal social life.
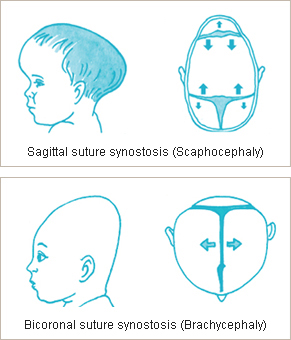
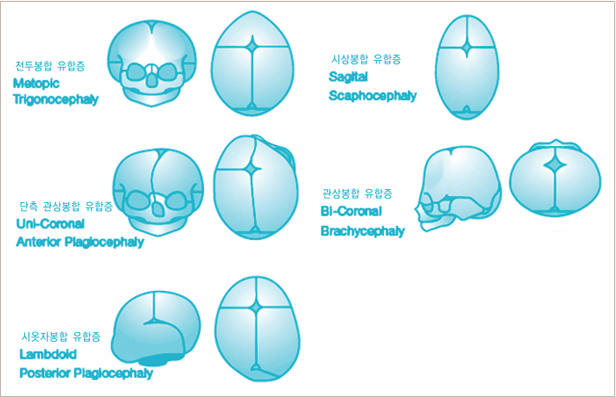
DiagnosisAccording to the location, cranial suture lines can be classified as the sagittal suture (the suture uniting the two parietal bones or the suture line of junction of parietal bones ), coronal suture (the suture between the parietal and frontal bones of the skull), frontal suture (the suture between two halves of the frontal bone), occipital suture (the suture on the hind part of the head, between the vertex and occiput dorsally), metopic suture (the suture line of junction of two halves of frontal bone), lambdoid suture (the suture line of junction between parietal and occipital bones) and craniosynostosis is clinically manifested and has a characteristic deformity according to the location of the sutures that are synostoed. If multiple suture lines are involved, developmental delay, visual disturbance, proptosis (protrusion of the eyeball), auditory dysfunction, respiratory failure, and seizure may be the critical symptoms. Other congenital anomalies like hydrocephalus, congenital anomaly of heart, lip, palate and hand may be accompanied. However, if only the single suture line is involved and there is no severe symptom, it cannot be easily detected and diagnosed. Differential diagnosis should be made from the acquired conformational deformity that results from the lying in one side for long time. Radiologic examination with simple X-ray, CT scan, and radionuclide imaging could be helpful for diagnosis.
Types of craniosynostosis
Crouzon’s syndrome
Apert’s syndrome
Appropriate timing of treatment If there is a sign of increased intracranial pressure (IICP), early surgical intervention is mandatory. In these situations, cranioplasty with the purpose of decreasing the cranial pressure before 3 months of age is needed. Without the sign of IICP or proptosis, surgery is planned around the age of 1. With the technical development, the timing of surgical intervention can be extended into the age of 2 to 3 years old.
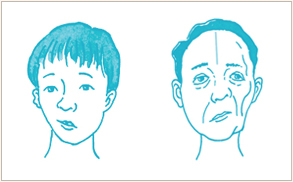
Asymmetric faceAlthogh there is no one that has exactly symmetric face, consultation to the plastic surgeon is mandatory if one has apparently asymmetric face at a glance. If the skeletal structure is distorted, one cannot give the feeling of beauty despite of attractive eye, nose, and mouth. One can make an examination by oneself with photograph. Look at the photo and make a close investigation whether the center of the eye, nose, and mouth is in accordance with each other. Look at the mirror and make sure that the midline of the central incisors is concordant with the central line of the face. One can be suspicious of asymmetric face when they bite the straight material such as chopstick and it reveals the non-horizontal figure on the mirror.
Etiology
Timing of treatment It takes long time to treat the hemifacial microsomia because it is complicated and time-consuming. Orthodontic treatment, orthognathic surgery, skin and soft tissue correction should be coordinated step by step for long therapeutic period. In severe cases, correction of the shape of the lip at the age of 1 to 2, reconstruction of the temporomandibular joint and external ear, orthognathic surgery at the adolescent period should be performed in order and finally facial contouring is considered in the adult age. Recently, distraction osteogenesis can be tried as well. However, if the symptom is not severe, surgical intervention should be planned after the age of 18 when the facial growth is completed. If the surgery is performed before the facial growth ends, additional surgical procedure may be needed after the completion of the skeletal development.
Surgical optionsAlmost all possible surgical skills imagined in the field of plastic surgery could be brought into the treatment of facial asymmetry. Orthognathic surgery, bone graft, distraction osteogenesis, flap surgery, and fat graft can be the options for the correction of the asymmetric face. If there is malocclusion or irregularities of teeth, orthodontic treatment is mandatory. Partial absorbance can be the problematic issue on using the autogenous tissue such as bone graft and fat graft that may result in the repetitive procedures. Several days of hospitalization and general anesthesia are necessary in most of the cases.
|
||
- Previous
- Orthognathic Surgery
- Next
- Clinic for Head & Neck Reconstruction